549 Canadians are diagnosed with diabetes every day, adding to the more than 5.7 million Canadians already living with disease. Diabetes rates in Canada continue to climb with no signs of levelling off.

A common misconception is that people with diabetes are more likely to have cavities because they have higher glucose levels in their saliva. While this can be true in some cases, it isn’t for those who are mindful of their oral health routines. After all, someone with diabetes is more likely to monitor their sugar intake and therefore don’t expose their teeth to as much sugary food. You can safely manage your oral health by visiting your dentist every 3-6 months if you have been diagnosed with diabetes. If you don’t, you may be at a higher risk for one of these conditions or diseases.
Diabetes and Dental Care Risks
Your dental clinic may be able to spot the signs of diabetes before your doctor does. This is because many patients will suffer from dry mouth and other conditions due to a decrease in saliva. Saliva is what keeps your mouth healthy with its pH buffering ability. Here’s what can happen if your diabetes and dental care routine go unchecked.
More prone to cavities.
It may be unpleasant to think about, but your mouth is the home to many microorganisms that interact with your saliva, food, and teeth. When some of these bacteria are combined with sugars, acidic foods or beverages, and carbohydrates, they produce a sticky film that covers your teeth. This is known as plaque.
If left for too long, the plaque will begin to attack your enamel and dentin, demineralizing your enamel. The higher your blood sugar levels, the more acid that causes tooth decay will be present.
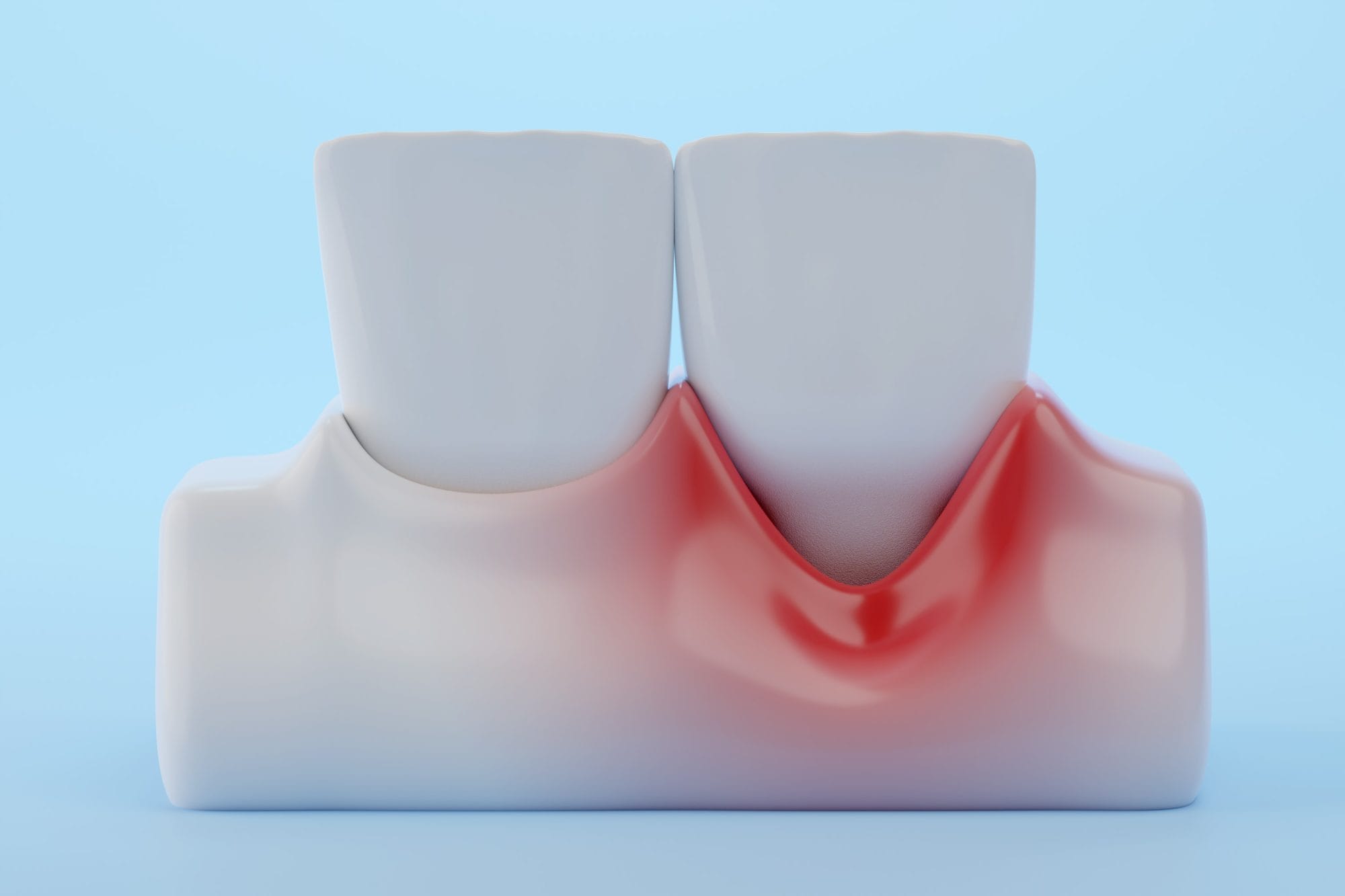
Gum disease.
Gum disease can vary from a mild inflammation to periodontitis. Periodontitis is the irreversible loss of bone around your teeth. When it starts, you may notice that your gums are swollen, turning red instead of their usual pink, and have a tendency to bleed more easily and often. It is not normal for your gums to bleed while flossing! Patients with diabetes who don’t have their blood sugar under control have more sugar in their saliva, which the bacteria will thrive on. Left unmonitored, the bacteria can promote plaque, which leads to further tooth decay and gum disease.
Thrush.
Thrush is a fungal infection caused by a particular group of yeast called Candida. It’s not contagious but can cause painful white or red patches in your mouth. The best defence against this infection is proper brushing and flossing practices. This is especially true for patients with diabetes who take antibiotics to fight infections since their body often takes longer to recover due to the disease.
Dry mouth.
As we’ve mentioned, saliva plays a crucial part in the overall health of your mouth. It helps buffer acids produced by bacteria in your mouth to prevent decay. However, high blood sugar can lead to frequent urination, which causes dehydration. This means there’s less water available in your body to make saliva. Decreased saliva leads to a dry mouth, and dry mouth can cause a burning sensation, ulcers, further tooth decay, and gum disease.
Slower healing time.
You’ll want to take excellent care of your oral health if you have diabetes. This is because patients with diabetes are at a higher risk of infection and often heal slower than someone who doesn’t have the disease. If necessary, your dentist may prescribe antibiotics to prevent or treat dental infections. However, antibiotics can also lead to thrush, which is why you’ll want to focus on prevention rather than treatment.
Tips to Manage Your Oral Health with Diabetes
Prevention is the best medicine for your oral health. You can take several steps to keep your teeth and gums healthy for years to come. Your daily routine should include:
- Brushing a minimum of twice per day. You should also check your toothpaste to ensure it includes fluoride for the best oral care. A high fluoride toothpaste like CTX4 5000 by Carifree is a great option for cavity prevention.
- Flossing at least once a day.
- Limiting sugary, starchy, sticky or acidic foods and drinks.
- Have your teeth professionally cleaned every 3-4 months. Patients with diabetes are at a higher risk of periodontitis. Removing the bacterial biofilm from your teeth more frequently helps lower inflammation and prevent progression of bone loss around your teeth.
- Managing your blood sugar levels. In general, a healthy person should aim for blood sugar levels between 5-8 mmol/L. However, in the elderly there are greater risks for hypoglycemia and you should talk to your doctor about your specific circumstances.
If you have been diagnosed with diabetes, your dentist may also work with you and your doctor when booking dental procedures to ensure your blood sugar is in check to avoid unnecessary infection or complications. It’s important that you do self-checks for any early signs of gum disease or tooth decay, as people with diabetes can experience them more often. If you’ve had a diabetes diagnosis and want to speak with a dentist who can help you develop a customized prevention plan, contact us now to book an appointment.
What surprised you about diabetes and dental care? Do you have any tips for excellent oral care? Share your comments with our readers who want to learn more.